Seasonal Affective Disorder: Understanding Winter Depression and Treatment Options
Seasonal affective disorder (SAD) is a type of depression that follows a seasonal pattern, most commonly emerging during the fall and winter months when daylight hours decrease. Known also as winter depression, SAD affects millions of people each year, causing significant changes in mood, energy, sleep, and appetite that can disrupt daily life. Understanding the symptoms, causes, and treatment options for seasonal affective disorder is essential for managing this condition effectively. In this article, we explore the key aspects of SAD, including how it is diagnosed, who is at risk, and the evidence-based therapies available to help individuals regain balance and well-being throughout the year.
Key Takeaways
What Is Seasonal Affective Disorder?
Seasonal affective disorder sad represents a subtype of major depression characterized by recurrent depressive episodes that occur during specific seasons year after year. This mood disorder affects approximately 5% of U.S. adults annually, with symptoms reliably appearing and disappearing in predictable seasonal patterns. Unlike occasional “winter blues,” seasonal affective disorder meets full clinical criteria for major depression and significantly impairs daily functioning.
The connection between reduced sunlight exposure and mood changes forms the foundation of how we understand this mental health condition. During fall and winter months, shorter daylight hours and decreased light intensity disrupt our brain’s natural circadian rhythm, leading to changes in brain chemicals that regulate mood, sleep, and appetite.
SAD occurs in two distinct patterns. Winter-pattern seasonal affective disorder, also called winter depression, typically begins in late fall or early winter and remits in spring and summer months. This represents the vast majority of cases. Summer-pattern SAD, called summer depression, is less common and occurs from late spring through early fall, resolving during winter months.
To diagnose seasonal affective disorder, mental health professionals look for depressive episodes that occur during specific seasons for at least two consecutive years, with full remission during off-seasons. The seasonal episodes must significantly outnumber any nonseasonal depressive episodes throughout the person’s lifetime.
At Ezra Counseling, we recognize that seasonal affective disorder represents a complex interaction between biological vulnerability and environmental triggers. Our comprehensive approach addresses both the neurobiological aspects of SAD and the psychological patterns that can develop around seasonal changes.
Recognizing SAD Symptoms
Understanding sad symptoms requires recognizing that seasonal affective disorder includes all core features of depression while presenting distinct seasonal characteristics. Symptoms must persist for at least 4-5 consecutive months annually and occur during about the same times each year to meet diagnostic criteria.
The severity of seasonal affective symptoms exists on a continuum. Some individuals experience mild seasonal mood changes that slightly impact functioning, while others develop debilitating depression requiring immediate intervention. A thorough evaluation by a mental health professional helps determine where someone falls on this spectrum and what level of treatment might be most beneficial.
Winter-Pattern SAD Symptoms
Winter depression typically begins in October or November and improves in March or April. The hallmark features distinguish it from other mental health conditions through their seasonal timing and specific symptom cluster.
Sleep patterns change dramatically during sad episodes. Many people experience hypersomnia, sleeping 9-12 hours per day yet still feeling fatigued and unrefreshed. This contrasts with the trouble sleeping seen in typical major depression. Alongside extended sleep, individuals often report feeling like they want to “hibernate,” withdrawing from social activities and reducing engagement in work or leisure pursuits.
Appetite and weight changes follow predictable patterns in winter-pattern seasonal affective disorder. Intense carbohydrate cravings and increased appetite commonly lead to weight gain during winter months. People often describe feeling unable to control their desire for sugary and starchy foods, which temporarily improve mood but contribute to feelings of guilt and physical discomfort.
Energy levels plummet during sad episodes, with many clients describing “leaden paralysis” – a heavy feeling in their arms and legs that makes movement feel difficult. This physical fatigue combines with mental fog and difficulty concentrating, impacting work performance and decision-making abilities.
Depression symptoms include persistent sadness, loss of interest in previously enjoyed activities, feelings of worthlessness, and in severe cases, thoughts of death or suicide. The seasonal pattern helps distinguish SAD from other mood disorders, but the depressive symptoms can be just as serious and debilitating.
Summer-Pattern SAD Symptoms
Summer depression presents differently from its winter counterpart, often surprising people who expect depression to occur during darker months. Summer sad typically begins in late spring and continues through early summer, resolving as days become shorter in fall.
Sleep patterns in summer depression involve insomnia or significantly reduced sleep needs. Rather than oversleeping, individuals may sleep only 4-6 hours nightly while feeling agitated and restless. This sleep disruption often contributes to irritability and difficulty managing stress during typically “happy” summer months.
Appetite changes in summer-pattern seasonal affective disorder involve decreased appetite and weight loss, opposite to winter depression patterns. Some people lose their interest in food entirely, while others feel nauseous or physically uncomfortable when trying to eat regular meals.
Anxiety and agitation characterize summer sad more than the sluggish feelings of winter depression. People may experience inner tension, increased irritability, and sometimes impulsive or aggressive behavior. The contrast between internal distress and external summer activities can create additional psychological stress.
Who Is At Risk for Seasonal Affective Disorder?
Demographic patterns reveal that seasonal affective disorder affects certain populations disproportionately. Women develop SAD at roughly four times the rate of men, similar to patterns seen in other mental health conditions like major depression and anxiety disorders. This gender difference may relate to hormonal influences on mood regulation and light sensitivity.
Age of onset typically occurs in young adulthood, with many people first experiencing seasonal depressive episodes between ages 18-30. However, seasonal affective disorder can develop during childhood and adolescence, and some individuals don’t develop SAD until later in life, particularly after major life changes or relocations to different climates.
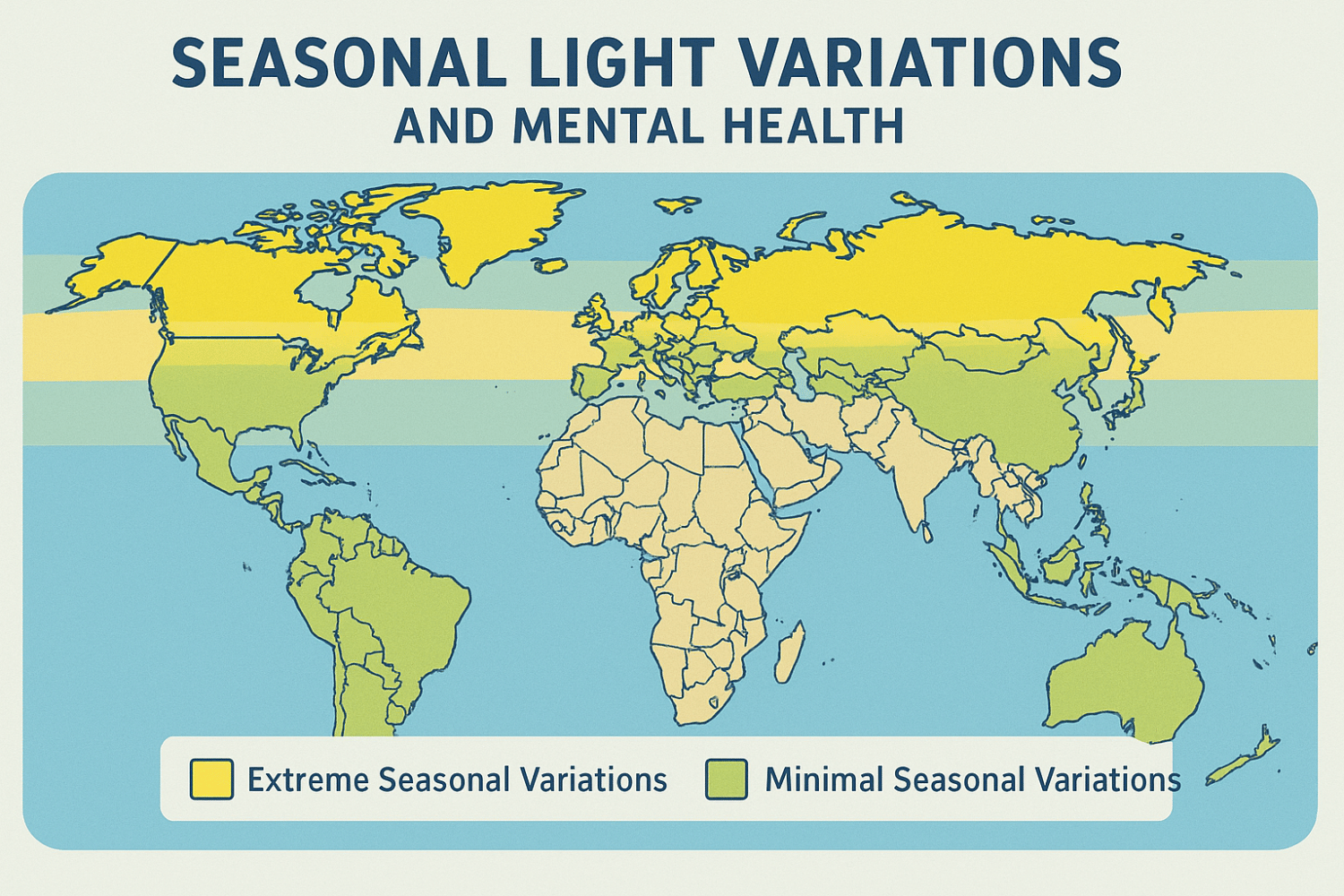
Geographic risk factors play a crucial role in who develops seasonal affective disorder. Prevalence increases significantly above 37 degrees north latitude, where winter daylight becomes markedly shorter. Residents of northern states like Maine, Vermont, and Washington experience SAD at rates up to 9-10%, compared to 1-2% in southern regions with less dramatic seasonal light changes.
Genetic predisposition contributes to seasonal affective disorder risk. People with family histories of depression, bipolar disorder, or other mental health conditions face increased vulnerability to developing SAD. Twin studies suggest hereditary factors interact with environmental light exposure to determine who develops seasonal mood problems.
Existing mental health conditions increase SAD risk substantially. Individuals with bipolar disorder commonly experience seasonal patterns in their mood episodes, requiring careful attention to prevent hypomanic or manic episodes when treating seasonal depression. Those with anxiety disorders, attention disorders, or eating disorders also show higher rates of seasonal mood changes.
At Ezra Counseling, we’ve observed that life circumstances can influence seasonal affective disorder development. People working in environments with limited natural light exposure, those with irregular schedules that disrupt circadian rhythms, and individuals with chronic medical conditions often show increased vulnerability to seasonal mood changes.
Understanding the Causes of SAD
The biological mechanisms underlying seasonal affective disorder involve complex interactions between light exposure, brain chemicals, and circadian rhythm regulation. Reduced sunlight during shorter days disrupts the brain’s internal clock, which normally coordinates sleep, hormone production, and mood regulation with the external light-dark cycle.
Serotonin activity plays a central role in seasonal depression development. During winter months, people vulnerable to SAD show reduced serotonin transporter binding and altered serotonin turnover in brain imaging studies. Less sunlight leads to decreased serotonin synthesis, contributing to the depressive symptoms characteristic of SAD. This explains why selective serotonin reuptake inhibitors prove effective for treating seasonal affective disorder.
Melatonin production becomes dysregulated in seasonal affective disorder. This hormone, secreted by the pineal gland during darkness, helps regulate sleep-wake cycles. In winter, longer nights and reduced daytime light alter melatonin secretion patterns, causing some people to produce too much melatonin for too long, contributing to oversleeping and daytime fatigue.
Circadian rhythm disruption represents a core mechanism in seasonal affective disorder development. The “phase-shift hypothesis” suggests that internal body clocks become misaligned with external light-dark cycles during winter. Without adequate morning light to anchor circadian rhythms, vulnerable individuals experience a chronic state similar to mild jet lag, manifesting as depressive symptoms.
Vitamin D deficiency may contribute to seasonal depression, particularly in northern climates where winter sun exposure becomes insufficient for adequate vitamin D synthesis. While not directly causative, low vitamin D levels often correlate with seasonal mood problems and may influence neurotransmitter function.
Psychological factors also influence how seasonal changes affect mood. Negative thoughts about winter, anticipatory anxiety about seasonal mood changes, and behavioral patterns of withdrawal can amplify biological vulnerability to seasonal affective disorder. Some people develop “seasonal identity” where they over-identify with SAD diagnosis, potentially creating self-fulfilling prophesies of winter impairment.
How Is SAD Diagnosed?
Diagnosing seasonal affective disorder requires a thorough evaluation by qualified mental health professionals who can distinguish SAD from other mental health conditions with similar symptoms. The diagnostic process involves comprehensive assessment of mood patterns, medical history, and functional impairment across multiple years.
The DSM-5 criteria for seasonal pattern specifier requires that major depressive episodes occur during specific seasons for at least two consecutive years, with full or nearly complete remission during off-seasons. Seasonal episodes must significantly outnumber any nonseasonal episodes throughout the person’s lifetime. This temporal pattern distinguishes SAD from major depression that coincidentally occurs during certain seasons.
Assessment tools help mental health professionals evaluate seasonal patterns systematically. The Seasonal Pattern Assessment Questionnaire (SPAQ) measures seasonal variations in sleep, social activity, mood, weight, appetite, and energy levels. While useful for screening, these questionnaires require clinical interpretation alongside thorough history-taking.
A thorough evaluation includes medical screening to rule out other conditions that might mimic or contribute to seasonal mood changes. Hypothyroidism, anemia, sleep apnea, chronic infections, and vitamin D deficiency can all cause fatigue, low mood, and cognitive difficulties that worsen during winter months. Basic laboratory tests often accompany initial SAD assessment.
Mental health professionals must carefully distinguish seasonal affective disorder from bipolar disorder with seasonal patterns. Many individuals with bipolar disorder experience winter depressions followed by spring or summer hypomanic episodes. Screening for past hypomanic symptoms – including periods of elevated mood, decreased sleep needs, increased energy, and impulsive behavior – helps determine whether someone has unipolar SAD or bipolar disorder with seasonal features.
At Ezra Counseling, our diagnostic approach emphasizes collaborative assessment where clients become partners in understanding their seasonal patterns. We help people track mood, energy, sleep, and functioning across seasons while exploring how environmental, social, and psychological factors interact with biological vulnerability.
Evidence-Based Treatment Options
Treating seasonal affective disorder effectively requires understanding that multiple approaches often work better than single interventions. Research demonstrates that combining light therapy, specialized psychotherapy, and when indicated, medication provides optimal outcomes for most people experiencing SAD.
The timeline for improvement varies depending on treatment modality and individual factors. Light therapy can produce noticeable benefits within 1-2 weeks, while antidepressant medications typically require 4-8 weeks to reach full effectiveness. Cognitive behavioral therapy provides both immediate coping strategies and longer-term skills for managing seasonal challenges.
Working with mental health professionals ensures treatment plans address individual needs, comorbid conditions, and personal preferences. Some clients prefer non-medication approaches, while others benefit from preventive medication started before symptoms emerge each year.
Light Therapy
Light therapy represents the most researched and widely recommended first-line treatment for winter depression. This treatment uses specialized light boxes that emit bright light to compensate for reduced natural sunlight exposure during shorter days.
Standard light therapy protocols use 10,000-lux light boxes positioned 16-24 inches from the user’s face for 20-30 minutes each morning. The timing matters significantly – morning light exposure works better than evening sessions for most people with winter-pattern seasonal affective disorder. Evening bright light can disrupt sleep and potentially worsen symptoms.
Research shows that when administered correctly, bright light therapy produces antidepressant effects comparable to standard medications for many people with seasonal affective disorder. Meta-analyses of controlled trials demonstrate response rates of 60-70% when light therapy is used consistently throughout fall and winter months.
Safety considerations make light therapy appropriate for most people, though certain precautions apply. Individuals with bipolar disorder, retinal conditions, or those taking medications that increase light sensitivity should use light therapy only under medical supervision. Common side effects include mild eyestrain, headache, or feeling slightly jittery, which usually resolve by adjusting distance or session length.
The key to light therapy effectiveness lies in consistency and proper technique. Users should keep their eyes open and oriented toward the light while engaging in other activities like reading or eating breakfast. Direct staring isn’t necessary and may cause discomfort. Treatment typically begins in early fall and continues daily until spring daylight consistently lengthens.
Cognitive Behavioral Therapy for SAD
Cognitive behavioral therapy tailored specifically for seasonal affective disorder (CBT-SAD) addresses both behavioral patterns and thinking styles that contribute to seasonal depression. This approach recognizes that while SAD has biological origins, psychological factors significantly influence how severely seasonal changes impact functioning.
CBT-SAD typically involves 6-12 weekly sessions that can be delivered individually or in group format. The therapy focuses on three main components: behavioral activation to counteract winter withdrawal patterns, cognitive restructuring to challenge negative seasonal thoughts, and relapse prevention to maintain gains across multiple winters.
Behavioral activation helps clients identify values-based activities that remain possible despite cold and darkness. Rather than hibernating during winter months, people learn to maintain social connections, physical activity, and meaningful pursuits through structured activity scheduling. This component directly combats the tendency to withdraw that characterizes winter depression.
The cognitive component examines automatic thoughts and beliefs about seasonal changes. Common maladaptive thoughts include “Every winter I fall apart,” “There’s nothing I can do about the darkness,” or “Winter ruins everything good in my life.” CBT-SAD helps people develop more balanced perspectives like “Winters are challenging for me, but I have specific tools that help.”
Research comparing CBT-SAD to light therapy shows both approaches provide significant benefit acutely. However, CBT-SAD may offer superior long-term outcomes with lower relapse rates in subsequent winters. This likely occurs because therapy provides lasting skills that people retain even after formal treatment ends.
At Ezra Counseling, we integrate CBT-SAD techniques with our broader therapeutic approach, helping clients develop personalized “winter wellness plans” that incorporate cognitive strategies, behavioral goals, and environmental modifications suited to their unique circumstances and values.
Antidepressant Medications
Selective serotonin reuptake inhibitors serve as first-line medication treatment for moderate to severe seasonal affective disorder. SSRIs like sertraline, fluoxetine, and citalopram have demonstrated effectiveness comparable to their use in nonseasonal major depression, with response rates typically ranging from 50-70%.
Bupropion extended-release holds unique FDA approval for preventing seasonal depressive episodes when started before symptoms begin each fall. Research shows that beginning bupropion XL in early autumn significantly reduces the likelihood of developing full depressive episodes compared to placebo. This preventive approach particularly benefits people with predictable, severe seasonal patterns.
Medication timing strategies depend on individual seasonal patterns and treatment goals. Some people prefer to start antidepressants when symptoms first emerge each fall, continuing through winter and tapering in spring. Others benefit from year-round treatment, especially if they experience nonseasonal mood symptoms or want to prevent any seasonal deterioration.
Side effect profiles for antidepressants used in seasonal affective disorder mirror their use in other mental health conditions. Common initial side effects include gastrointestinal upset, sleep changes, and sexual dysfunction. Most side effects diminish within 2-4 weeks as the body adjusts to medication. Close collaboration with prescribing physicians ensures optimal dosing and monitoring.
Combination approaches often prove most effective for seasonal affective disorder treatment. Many clients benefit from combining morning light therapy with antidepressant medication, particularly during initial treatment phases or for severe symptoms. The combination may allow for lower medication doses while maintaining therapeutic benefits.
Vitamin D Supplementation
Vitamin D supplementation represents an important adjunctive treatment for seasonal affective disorder, particularly given the high prevalence of vitamin D deficiency in northern climates during winter months. Research suggests that low vitamin D levels correlate with seasonal mood problems, though the exact causal relationship remains under investigation.
Healthcare providers typically recommend vitamin D3 (cholecalciferol) supplementation at doses ranging from 1,000-4,000 IU daily, depending on baseline blood levels and individual factors. A blood test measuring 25-hydroxyvitamin D levels helps determine appropriate dosing and monitors treatment response over time.
While vitamin D supplementation alone rarely resolves seasonal affective disorder, it can provide meaningful support as part of comprehensive treatment plans. Some research suggests that adequate vitamin D levels may enhance the effectiveness of other SAD treatments like light therapy and antidepressants.
Safety considerations include potential interactions with certain medications and the possibility of vitamin D toxicity at very high doses. Working with healthcare providers ensures appropriate monitoring and dosing adjustments based on individual response and blood levels.
Prevention and Self-Care Strategies
Preventing seasonal depressive episodes requires proactive planning that begins before symptoms typically emerge each year. People with histories of seasonal affective disorder benefit from implementing protective strategies in early fall, rather than waiting for depression symptoms to develop.
Sleep patterns form the foundation of seasonal wellness strategies. Maintaining consistent bedtimes and wake times, even on weekends, helps stabilize circadian rhythms that become vulnerable during seasonal transitions. Most adults need 7-9 hours of sleep nightly, and avoiding excessive sleep during weekends prevents the circadian drift common in seasonal depression.
Maximizing natural light exposure provides one of the simplest yet most effective prevention strategies. Even on overcast winter days, outdoor light intensity far exceeds typical indoor lighting. Scheduling daily outdoor activities, positioning workspaces near windows, and keeping curtains open during daylight hours all contribute to maintaining adequate light exposure.
Regular exercise serves multiple functions in preventing seasonal mood problems. Physical activity directly improves mood through endorphin release while also providing light exposure when conducted outdoors. Even moderate-intensity activities like brisk walking for 20-30 minutes daily can significantly impact seasonal mood symptoms.
Nutritional strategies focus on maintaining stable blood sugar and avoiding the extreme carbohydrate cravings that characterize seasonal depression. Well balanced meals that include complex carbohydrates, lean proteins, and healthy fats help regulate energy levels throughout the day. Limiting refined sugars and processed foods prevents the blood sugar fluctuations that can worsen mood symptoms.
Social support plays a crucial protective role against seasonal isolation. Maintaining regular contact with friends and family, scheduling social activities throughout winter months, and participating in community groups or activities helps counteract the withdrawal tendencies of seasonal depression.
Stress management techniques become particularly important during vulnerable seasons. Mindfulness meditation, deep breathing exercises, yoga, or other relaxation practices help manage the anxiety and tension that often accompany seasonal mood changes. Regular practice of stress reduction techniques builds resilience against seasonal challenges.
At Ezra Counseling, we work with clients to develop personalized prevention plans that incorporate these strategies based on individual preferences, schedules, and resources. These plans serve as roadmaps for navigating seasonal challenges while maintaining optimal mental health.
When to Seek Professional Help
Recognizing when seasonal mood changes require professional intervention can prevent minor difficulties from becoming major depressive episodes. Several warning signs indicate the need for immediate mental health support, particularly when symptoms persist for more than two weeks or significantly impact daily functioning.
Persistent hopelessness, thoughts of death or suicide, inability to perform work or family responsibilities, or severe social withdrawal all require prompt evaluation by mental health professionals. These symptoms indicate that seasonal changes have progressed beyond normal adjustment difficulties to clinically significant depression requiring treatment.
Early intervention provides the best outcomes for seasonal affective disorder. People who seek help at the first signs of seasonal mood changes often prevent full depressive episodes and maintain better functioning throughout challenging seasons. This proactive approach contrasts with waiting until symptoms become severe before seeking support.
The 988 Suicide and Crisis Lifeline provides immediate support for anyone experiencing thoughts of self-harm or suicide. This resource operates 24/7 and connects callers with trained counselors who can provide immediate safety planning and local resource referrals.
At Ezra Counseling, we maintain availability for urgent consultations when clients experience worsening seasonal symptoms. Our approach emphasizes early intervention and collaborative treatment planning that addresses both immediate symptom relief and long-term seasonal wellness strategies.
Insurance coverage for mental health services includes seasonal affective disorder treatment under mental health parity laws. Most insurance plans cover therapy, psychiatric evaluation, and when medically necessary, medication management for seasonal depression. Understanding coverage options helps remove barriers to accessing needed treatment.
Crisis resources extend beyond immediate safety to include community mental health centers, employee assistance programs, and university counseling services. These resources provide various levels of support depending on individual needs and circumstances.
Your Questions Answered
Can children and teenagers develop seasonal affective disorder?
Yes, seasonal affective disorder can develop during childhood and adolescence, though it’s more commonly diagnosed in young adulthood. Children may show different symptoms than adults, including increased irritability, difficulty concentrating at school, and changes in eating or sleeping patterns that follow seasonal cycles. Parents should consult with pediatric mental health professionals if they notice consistent seasonal mood changes that impact their child’s functioning across multiple years.
How long does it typically take to see improvement with SAD treatment?
Treatment response timelines vary by intervention type. Light therapy often produces noticeable improvements within 1-2 weeks of consistent use, while the full benefits may take 4-6 weeks. Antidepressant medications typically require 4-8 weeks to reach full effectiveness, though some people notice initial improvements within 2-3 weeks. Cognitive behavioral therapy provides some immediate coping strategies while building longer-term skills over 6-12 sessions. Combination treatments may accelerate improvement compared to single interventions.
Is it possible to have both summer and winter pattern SAD?
While uncommon, some individuals do experience mood difficulties during both seasonal transitions, though typically one pattern predominates. More often, people with year-round mood disorders may notice seasonal worsening during specific times. This pattern requires careful evaluation to distinguish from bipolar disorder or chronic depression with seasonal variations. Treatment approaches must be tailored to address the specific pattern and underlying mood disorder.
Can moving to a sunnier climate cure seasonal affective disorder?
Geographic relocation can reduce seasonal affective disorder symptoms for some people, particularly those moving from very northern latitudes to areas with more consistent daylight year-round. However, SAD isn’t simply cured by climate change, as the disorder involves complex biological and psychological factors beyond light exposure alone. Additionally, summer-pattern SAD might actually worsen in consistently sunny climates. Professional evaluation helps determine whether relocation might be beneficial and what other treatments should continue.
What should I do if my seasonal depression symptoms are getting worse despite treatment?
Worsening symptoms during treatment require immediate consultation with your mental health professional. This could indicate need for treatment adjustments, such as increasing light therapy duration, medication dosage changes, or adding additional therapeutic modalities. Sometimes symptoms temporarily worsen before improving, particularly in early treatment phases. However, any thoughts of self-harm, inability to function, or severe hopelessness warrant urgent professional evaluation and possible crisis intervention services.